Empathy is essential for interpersonal helping and is considered a key change process in psychotherapy (1). To empathise with another is to see things from their perspective and to feel with them, or to use the metaphors ‘to walk in their shoes’ or to ‘look from their window’. It is widely understood and defined as “… the action of understanding, being aware of, being sensitive to, and vicariously experiencing the feelings, thoughts, and experience of another of either the past or present without having the feelings, thoughts, and experience fully communicated in an objectively explicit manner” (2). Empathy connotes more than a sympathetic relating to another person’s observed mental state or the automatic mirroring of contagious emotion whether sorrow, fear or triumph (3). Empathy is a deliberate rather than passive process and involves perceptual, cognitive, emotional regulation and communicative processes. To be usefully employed in the process of helping, an empathic understanding of another’s experience (including thoughts and feelings) needs to be communicated back to the person in a congruent, non-judgemental way which makes a difference to them. Indeed, it is this communication of understanding this sense of being not only heard but understood that makes empathy so powerful. Everyone wants to be understood!

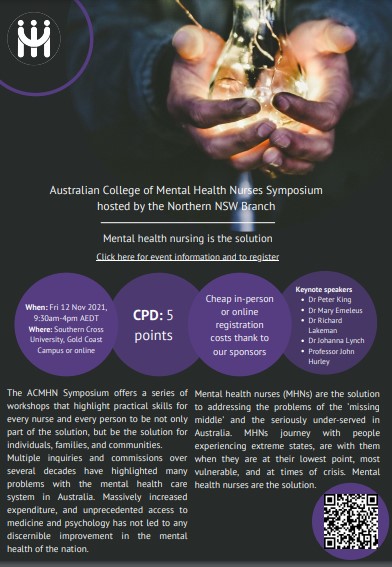
Over the years I
have been involved in organising and presenting at many conferences. In
particular I was involved in organising many symposia under the auspices
of the then 'Australian and New Zealand College of Mental Health
Nurses'. Recent career highlights have included presenting at a mental
health recovery conference in Bern, and the 40th Anniversary Conference
of the Australian College of Mental Health Nurses. I was very pleased to
have been the convenor of the 2007, Health4Life conference
in Dublin at which Tom Szasz was amongst many special guests (pictured).
Some papers are available for
download in text or video. Click on the
![]()
![]()
![]() icons
if available.
icons
if available.