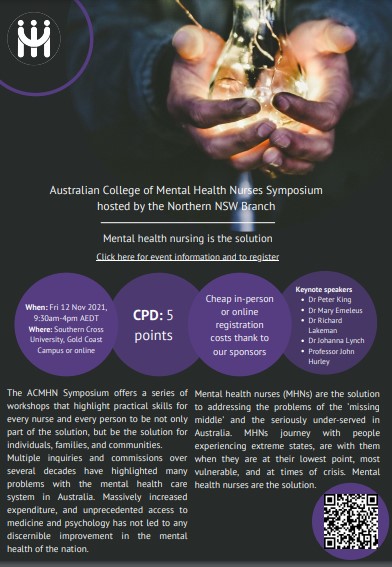
In 2023 the Australian Therapeutic Goods Administration approved the limited prescription of psilocybin and MDMA by psychiatrists in specific circumstances. This offers potential relief for many people suffering severe, enduring, complex and “treatment resistant” distress associated with post-traumatic stress disorder and intractable depression. It further offers opportunities for psychotherapists who wish to develop skills and apply existing skills in this specialized niche field of practice. Mental Health Nurses are well poised to take advantage of the possibilities offered by psychedelic-assisted therapies for a number of reasons we will discuss.
The use of psychedelics to enhance consciousnes
s and as ‘mind medicine’ has thousands of years of history. In traditional societies and enduring cultures, psychedelics have been used safely in the context of careful preparation, rituals and ceremonies and oversite by elders and experts. While it is tempting to be distracted by the ‘psychedelic experience’ inherent in the use of these medicines, we make the point that the experience itself is of limited value unless embedded in a safe, skilful, and well-informed setting in which a therapeutic context is vital (Lakeman, Emeleus & Ryan, 2023). Indeed most research into the medical use of psychedelics has incorporated hours of psychotherapeutic preparation, supervised dosing and crucially extensive post-dosing integration. That context provides the opportunity for people to ‘reset’ previous maladaptive or self-defeating modes of thinking but that does not happen purely as a result of ingesting psychedelic substances. It is an outcome of skilled therapy assisted by those substances.
This presentation will briefly address some of the history, significant evidence, research and practice base for the mechanisms of action and the use of psychedelic-assisted psychotherapy. We will outline the clinical settings and practice skills desirable to facilitate change using the medicines, with an emphasis on practice relevance for mental health nursing and some thoughts about future directions.
Lakeman, R., Emeleus, M., Ryan, T. (2023). It's not and never has been just the drug: The need to emphasize psychotherapy in psychedelic-assisted psychotherapy [Letter], International Journal of Mental Health Nursing, Early View.







.jpg)